Overview
OverviewIf the joint on one of your toes, usually the toe next to the big toe or the smallest toe, points upward rather than lying flat, you might have a Hammertoe. The condition is actually a deformity that happens when one of the toe muscles becomes weak and puts pressure on the toe?s tendons and joints. This pressure forces the toe to become misshapen and stick up at the joint. Also, there?s frequently a corn or callus on top of the deformed toe. This outgrowth can cause pain when it rubs against the shoe.
Causes
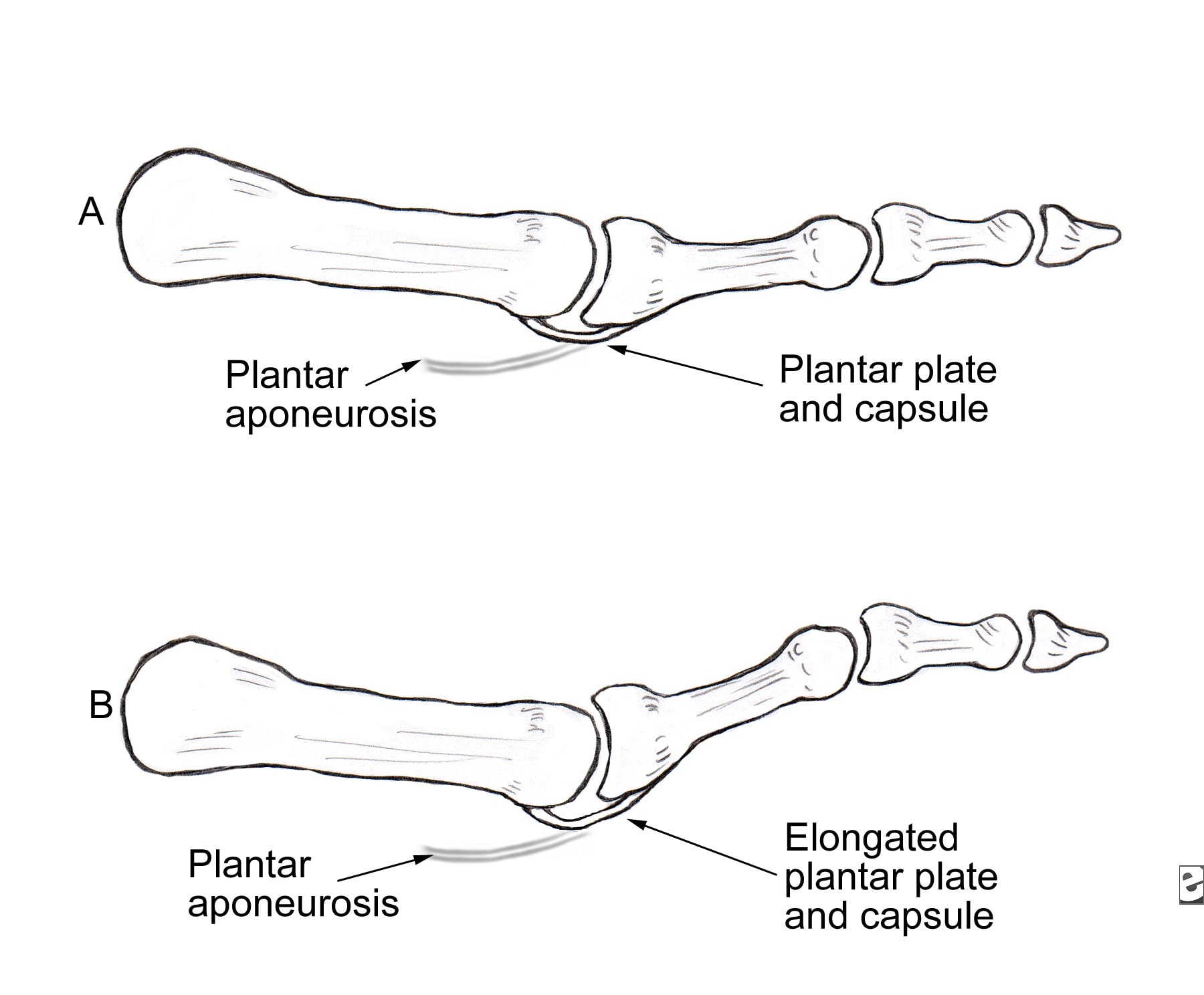
Some causes of hammertoe are shoes that are too tight or short, shoes with high heels, injury, Diseases that affect the nerves and muscles, such as arthritis and diabetes. When shoes do not fit well, over time the pressure of the shoes pushes the toes into a bent position. After a while, the muscles become unable to straighten the toe, even when you are not wearing shoes. Similarly, when there is damage or disease of the nerves or muscles in the toes, the toe may rest in the bent position until the tendons become permanently shortened and the toe becomes a rigid hammertoe. The risk of developing a hammertoe increases with age. Women are much more likely to develop a hammertoe than men.
Symptoms
The most obvious symptom of hammer, claw or mallet toe is the abnormal toe position. This is usually combined with pain: the abnormal foot position leads to excessive friction on the toe as it rubs against any footwear which can be extremely painful. Corns & Calluses: repeated friction can result in the formation of a foot corn or callus on top of the toes. Stiffness, the joints become increasingly stiff. In the early stages, the toes can usually be straightened out passively using your hands, but if allowed to progress, the stiffness may be permanent.
Diagnosis
Most health care professionals can diagnose hammertoe simply by examining your toes and feet. X-rays of the feet are not needed to diagnose hammertoe, but they may be useful to look for signs of some types of arthritis (such as rheumatoid arthritis) or other disorders that can cause hammertoe.
Non Surgical Treatment
Often padding and taping are the first steps in a treatment plan. Padding the hammer toe prominence minimizes pain and allows the patient to continue a normal, active life. Taping may change the imbalance around the toes and thus relieve the stress and pain. Anti-inflammatory drugs and cortisone injections can be prescribed to ease acute pain and inflammation caused by the joint deformity. Custom shoe inserts made by your podiatrist may be useful in controlling foot function. An orthotic device may reduce symptoms and prevent the worsening of the hammer toe deformity.
Surgical Treatment
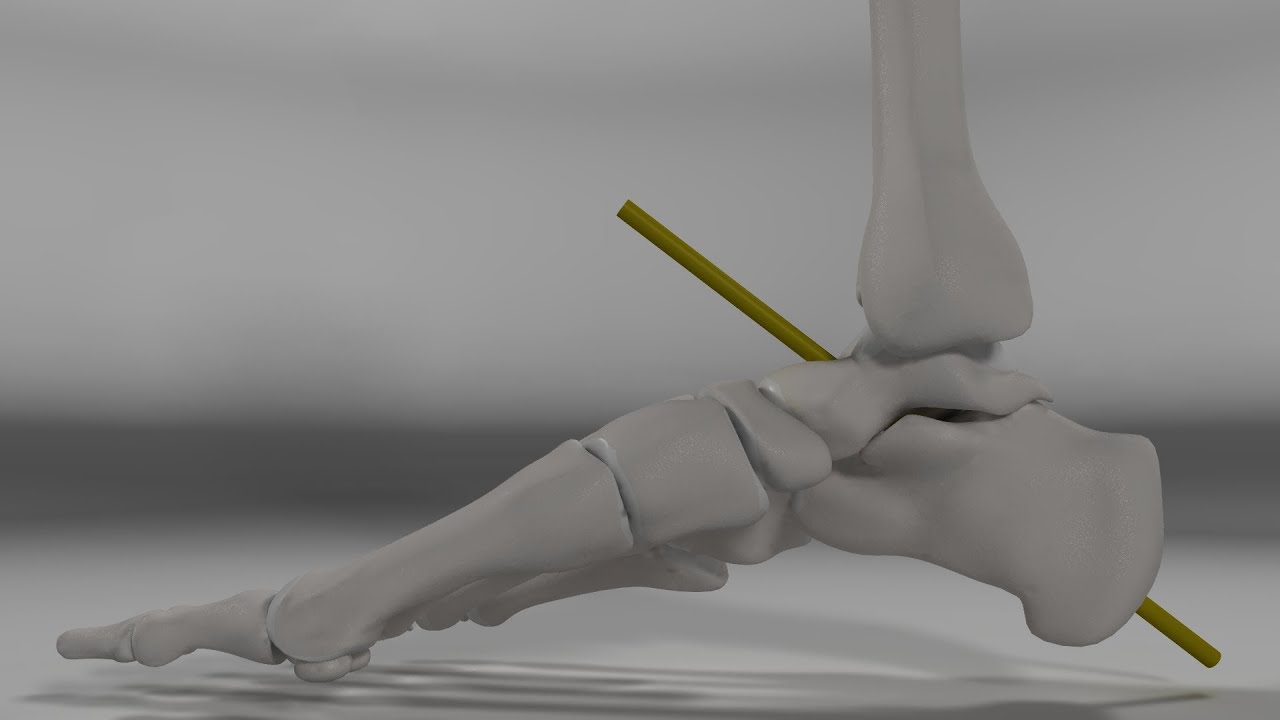
Surgery is the approach that is often necessary to correct hammertoe that fails to respond to nonsurgical management. Surgery is appropriate when the muscles and tendons involved in a hammertoe problem have become so tight that the joints are rigid, misaligned and unmovable. There are a number of surgical techniques for dealing with the complex range of joint, bone, muscle, tendon and ligament abnormalities that define each hammertoe's make-up. To correct a hammertoe deformity, the surgeon's goal is to restore the normal alignment of the toe joint, relieving the pressure that led to the hammertoe's development (this should also relieve the pain, as well). To do this, he or she may remove part of the boney structure that creates a prominence at the top of the joint. Tighten or loosen the muscles, tendons and ligaments around the toe joints. Realign the toe bones by cutting one or more and shifting their position, realigning muscles, tendons and ligaments accordingly. Use screws, wires or plates to hold the joint surfaces together until they heal. Reconstruct a badly damaged joint or replace it with an artificial implant.

Prevention
The number-one hammertoe prevention tip is to wear properly fitting shoes. If your shoes feel too snug, go to your local shoe store and have the length and width of your feet measured. If you wear high heels, keep the heel height to 2 inches or less. Wearing shoes with high heels increases the pressure on your toes and causes them to bend. It can also cause the formation of corns and a high arch.